Addictions and Substance Use
This blog post is associated with episode nine of the podcast with Mike Pond, a psychotherapist who had battled with alcohol use disorder. He lost his practice, home, and family. He floated through recovery homes, was dumpster diving, and was in prison because of his challenges with alcohol. To learn more about his story, I invite you to read his book and to watch his documentary.
“Just one drink!”
“Why can’t you just stop? It’s so easy.”
“I’m so hungover, I don’t want to work today.”
“I can’t wait to get high.”
“I need to hide this from my partner, friends, and family.”
“I can barely remember what happened last night.”
“I don’t want to be a party pooper..I’ll just have one…”
Drug and alcohol use has become more prevalent over the past few decades because of the increased accessibility and that they are used in numerous social settings, which has normalized it. Conversely, because it’s much more common, it has also created a huge negative stigma on people who are experiencing challenges with reducing or quitting. Many individuals feel embarrassed, ashamed, and guilty about their substance use because it’s seen as something that can be easily controlled with willpower.
“My friend only has one drink when we’re at happy hour, why can’t I? There must be something wrong with me.”
In the DSM-5 (Diagnostic and Statistical Manual of Mental Disorders, 5th Edition), substance use disorders (SUD) are recognized as disorders resulting from using drugs, alcohol, caffeine, cannabis, inhalants, opioids, stimulants, tobacco, or other substances. When you consume a substance, it causes the brain’s reward system to release dopamine and endorphins, causing you to feel a wave of euphoria, or that “high.” In turn, this can eventually lead to the development of urges and cravings to have another drink or dose of the substance of choice. Your brain and body become used to wanting this “high” and it can eventually lead to an addiction.

Some of the criteria include:
Some statistics to consider:

While many individuals develop a substance use disorder due to social circumstances such as falling into a habit of getting high or drinking after work, celebrating something, or for a stressful day, some use it as a coping mechanism to alleviate physical and emotional pain. For others, if substance use was present in their family history, it could be passed down genetically. Not only that, but their environment or how they grew up around substances could vary too. Perhaps they had a traumatic childhood or a parent or loved one was using it heavily. Each person has a different set of circumstances that create challenges for them. As a result, treatment will vary for each person as well.
In 1977, James Prochaska and Carlo Di Clemente developed the process of change model, which is often used to describe the stages of overcoming addiction or other behaviours that individuals are looking to change. It moves away from being confrontational and judgemental as it incorporates more person-centred and motivational attitudes. While the stages go in a cycle, individuals may start at different stages, jump between them, or go forward or backwards. This reaffirms the notion that change varies from person to person depending on their situation or environment.
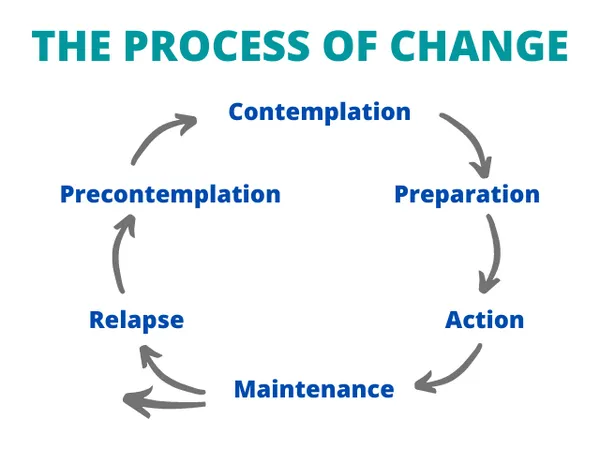
Precontemplation stage: The first stage of change in the addictions model where individuals do not acknowledge or think of their behaviours as an addiction. They might be in denial or have not had negative consequences occur as a result of their behaviours.
Contemplation: People might be in this stage for many years before taking action. They are considering treatment options or resources and are more receptive to receiving this information.
Preparation: During this stage, individuals are taking steps by determining what kind of change they want to make, how to make the change, speaking with others about it to develop a support system, and tapping into treatment options.
Action: Individuals are engaged in some form of treatment such as therapy, inpatient or outpatient programs, or using strategies to limit their triggers and cravings.
Maintenance: Individuals have met their goals for reduction or abstinence and are working to keep their behaviours out of the addictive loop. This is the most challenging stage because motivation levels are lower compared to the action stage and changes in their lives can impact their behaviours.
Relapse: This can happen in varying magnitudes with the individual engaging in the addictive behaviour again. They may go back into the previous stages as a result and undergo the process of change again.

Outside of the traditional inpatient programs which can cost up to $30,000 and often lack evidence-based approaches, individuals can consider other treatment options for substance use disorders such as:

Most importantly, be kind to yourself. Creating new habits or changing addictive behaviour is not easy and you are not alone in this. If you or a loved one may be experiencing challenges with substance use or addictive behaviour, I encourage you to consider one tangible step to create change or show support.